Breast cancer is the second most common cause of cancer death in women, surpassed only by lung cancer. For women aged 45 to 55, it is the No. 1 cause of death overall. Every year approximately 205,000 women are diagnosed with breast cancer, and of these, more than 40,000 will die. Studies have shown repeatedly that the best way to beat any type of cancer is through early and proper diagnosis, but new guidelines for breast health screenings call for delays in these procedures. With early diagnosis being so vital to the success of treatment and higher survival rates, this could be problematic.
.
Recent Changes in Cancer Screening Protocols
The new recommended protocols include the following:
- Routine screening of average-risk women should begin at age 50, instead of age 40.
- Routine screening should end at age 74.
- Women should get screening mammograms every two years instead of every year.
- Breast self-exams are unimportant because they have little value, based on findings from several large studies.
These recommendations come from the U.S. Preventive Services Task Force, a group of independent health experts put together by the Department of Health and Human Services. These new protocols have introduced confusion and concern for both medical professionals and affected women. Part of the confusion comes because the American Cancer Society still recommends annual screening for all healthy women beginning at age 40.
Concerns with New Cancer Screening Guidelines
One of the biggest concerns with the new guidelines is whether insurance will still cover routine screenings for women ages 40-49. Skipping these early screenings can have dire consequences for early detection and treatment. According to studies in the Archives of Internal Medicine, 6 percent to 16 percent of women with breast cancer experienced physician-caused delays in diagnosis. This suggests that at least 10,000 of the approximately 180,000 women diagnosed as having breast cancer each year experience treatment delays because of misinterpretation or misapplication of tests. The fear is the new guidelines will make obtaining screening mammograms more difficult and costly for patients, compounding an already-disturbing risk of misdiagnosis.
Coping with these Increased Risks
Even with timely screenings, patients are still subject to an array of errors that can cause untold pain, suffering and even death. When doctors fail to request mammograms when patients present with persistent and palpable breast lumps, this leads to treatment delay. Cancer is often missed when medical professionals fail to properly interpret mammograms. Additional misdiagnoses occur when inadequate or inaccurate sampling of breast tissue is acquired during biopsy or when mismatched pathology specimens lead to missing critical cancer indications.
In many cases, physicians continue to inappropriately reassure patients that masses are benign, even without biopsy. The fear is that, with the new recommendations, doctors will be even less willing to prescribe screening or further diagnostics. Although these guidelines are not federal policy and do not prohibit women 40-49 from getting mammograms, many fail to do so because their doctors claim it’s not necessary.
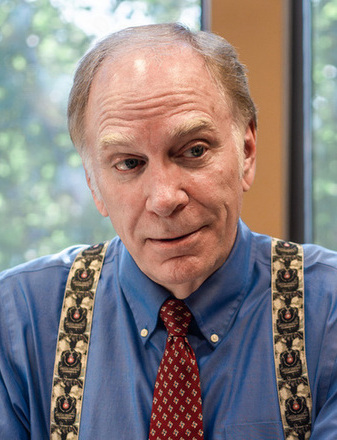
If you or a loved one suspects that a diagnosis of breast cancer was missed or delayed due to misinterpreted X-rays, lack of screening or poorly performed testing, contact Rasmussen and Miner today. Some cancers are virulent and grow much faster, so much so that even short delays will likely have a greater adverse effect on outcomes. If you have questions or doubts about the medical explanations your physician has given you, we would like to speak with you about your concerns related to breast cancer.